No birth control method is 100% effective. Whether it’s a missed pill, a broken condom, or a late shot, birth control failure can happen. If you’re concerned about the possibility of an unintended pregnancy or a sexually transmitted infection (STI) due to contraceptive failure, knowing the next steps of birth control fails is essential for your health and peace of mind.
Understand What “Birth Control Failure” Means
No Method Is Foolproof
Even the most effective contraceptive methods come with a small risk of failure:
Birth control pills: 91% effective with typical use.
Condoms: 85% effective with typical use.
IUDs: Over 99% effective but still carry a rare risk of failure.
Implants and shots: Very effective, but not infallible.
Failure can result from user error, product defects, or interactions with medications (especially antibiotics and certain herbal supplements like St. John’s Wort).
Step 1: Stay Calm and Assess the Situation
Take a Deep Breath
It’s natural to feel worried, anxious, or overwhelmed. But try to remain calm so you can evaluate the situation clearly.
Identify the Type of Failure
Ask yourself:
Was the condom broken or slipped off?
Did you miss a pill or take it late?
Did the patch fall off or the ring come out?
Has your birth control injection expired?
Did you have unprotected sex while off schedule?
Understanding the type of failure helps determine the next best step.
Step 2: Consider Emergency Contraception
What Is Emergency Contraception?
Emergency contraception (EC) helps prevent pregnancy after unprotected sex or contraceptive failure. It works best the sooner it’s taken.
Types of Emergency Contraception
Morning-After Pills
Levonorgestrel (Plan B One-Step and generics): Available over-the-counter; most effective within 72 hours.
Ulipristal acetate (ella): Prescription-only; effective up to 5 days after sex.
Copper IUD (Paragard)
The most effective form of EC.
Can be inserted by a healthcare provider within 5 days of unprotected sex.
Provides ongoing contraception for up to 10+ years.
Who Should Consider EC?
You should consider emergency contraception if:
- You missed two or more birth control pills.
- A condom broke or wasn’t used.
- Your patch or ring was out for too long.
- You were relying on withdrawal (which has a high failure rate).
- You’re unsure about your contraception status.
Step 3: Monitor for Early Signs of Pregnancy
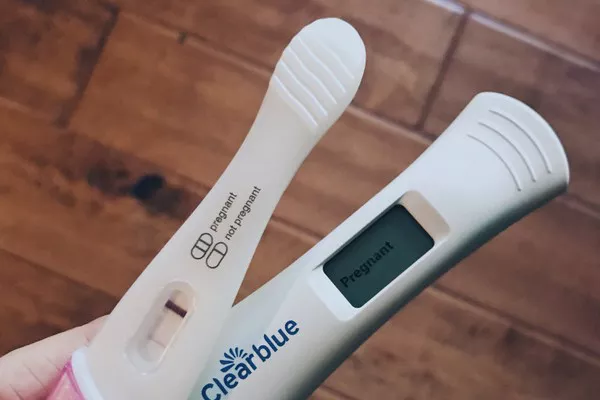
When to Take a Pregnancy Test
If you suspect birth control failure, wait at least 10 to 14 days after the incident before taking a home pregnancy test for accurate results. Alternatively, wait until the first day of a missed period.
Early Symptoms to Watch
- Missed or delayed period
- Breast tenderness
- Fatigue
- Nausea
- Spotting or light cramping
These signs can also result from hormonal fluctuations, so testing is the only reliable way to confirm pregnancy.
Step 4: Schedule a Medical Appointment
Talk to a Healthcare Provider
It’s important to check in with a doctor, nurse practitioner, or OB-GYN to:
- Confirm pregnancy (if applicable)
- Discuss long-term contraceptive options
- Screen for sexually transmitted infections (STIs)
- Talk through your concerns and next steps
Many clinics offer confidential services, especially for teens and young adults.
STI Testing
If your contraceptive failure involved a broken condom or unprotected sex with a new partner, STI testing is strongly recommended—even if you have no symptoms.
Step 5: Understand Your Options If Pregnancy Occurs
If You’re Pregnant
An unintended pregnancy can lead to a wide range of emotions—fear, confusion, hope, or even joy. Whatever you’re feeling is valid. You have three primary options:
1. Continue the Pregnancy
- Begin prenatal care as early as possible.
- Connect with an OB-GYN or midwife.
- Consider support from family, friends, or community resources.
2. Adoption
- If parenting isn’t the right path, but you choose to carry to term, adoption is an option.
- You can make a plan through agencies, private arrangements, or state services.
3. Abortion
- Legal access varies by location and state.
- Medical or surgical abortions are available based on gestational age and local laws.
- Consult a licensed provider or family planning clinic for safe and accurate information.
Step 6: Reflect and Reevaluate Your Birth Control Method
Was It the Right Method for You?
Sometimes failure happens because the method wasn’t ideal for your lifestyle. Questions to ask:
- Did you frequently forget to take pills?
- Was the method hard to maintain (e.g., replacing the ring or patch)?
- Do you want a more permanent or long-lasting solution?
Consider Long-Term Options
More effective or lower-maintenance methods include:
- IUDs (hormonal or copper)
- Implants (like Nexplanon)
- Birth control shot (Depo-Provera)
- Permanent options: Tubal ligation or vasectomy (for partners)
Talk to your provider to weigh the pros and cons of each method.
Step 7: Prioritize Emotional and Mental Well-Being
You Are Not Alone
Unexpected situations around birth control can be distressing. It’s okay to seek emotional support through:
- Friends or trusted family members
- Counselors or therapists
- Support groups
- Reproductive health hotlines
Remember, this is a common experience—millions of people face contraceptive failure at some point.
Conclusion
Birth control failure can be scary, but it doesn’t have to be overwhelming. By staying calm, acting quickly, and seeking support, you can take control of the situation and protect your health.
Whether you choose emergency contraception, reassess your birth control method, or navigate a potential pregnancy, know that medical professionals, support networks, and resources are available to help you every step of the way.
You Might Be Interested In:
- The Rise of “Pregnancy Pods”: How Virtual Support Groups Are Transforming Maternal Mental Health
- Climate Change and Pregnancy: New Study Links Air Pollution to Higher Risk of Premature Birth
- Breakthrough in Prenatal Testing: New Non-Invasive Method Detects Genetic Disorders Earlier